News
NGOs in Afghanistan Meet the Difficult Challenge of Reducing Maternal Mortality
- 22 August 2003
News
MAZAR-I-SHARIF, Afghanistan—The full waiting room at the Char Bolak clinic is clear sign that life is getting better in one northern village, thanks in part to a small non-governmental organization supported by UNFPA. Childbirth has become safer here since prenatal exams and supplies for clean home deliveries have become available.

A year ago many residents were returning from exile abroad, having fled the war, or from camps where they had gone to escape the effects of a drought. There was peace for the first time in 23 years and the rains had resumed, but the area had no health centres or trained medical staff.
The Medical Relief Unit (MeRU), a Japanese NGO set up to assist those displaced by the drought, shifted its focus to providing health care in poor villages lacking services. With funds and supplies provided by UNFPA, the United Nations Population Fund, and Afghan staff assigned by the Ministry of Health, MeRU opened maternal and child health clinics in borrowed homes in Char Bolak and a more remote village, Ahmad Abad, along with a better equipped referral centre in the city of Balkh.
Today, MeRU manages the three well-stocked facilities and is building new clinic buildings in Char Bolak and Ahmad Abad. For a small fee, the clinics provide prenatal exams, infant checkups and treatment for a variety of ailments.
A morning visit to the Char Bolak clinic finds a female doctor, a midwife, a pharmacist and a receptionist on duty. Women with children sit on one side of the waiting room; men and more children sit on the other. The patient logbook indicates the most common cases are diarrhoea and pneumonia. Mihoko Osawa, administrator for MeRU, checks progress on the new building, while the medical coordinator, Miwako Arai, a Japanese nurse, checks the medical supplies.
Ahmad Abad, a village of narrow, winding streets and mud and brick houses behind high mud walls, is a dusty, jolting, hour-long drive away. By the time a group of visitors arrives at the clinic, the waiting room is empty. It is nearly noon and 45 degrees (113 degrees Fahrenheit); in summer, clients come early in the morning. Inside, the head doctor, Dr. Walid, examines a small boy on his mother’s lap.
MeRU is one of 22 Afghan and international NGOs that UNFPA is partnering with in an effort to increase access to life-saving medical care. High maternal mortality is the most severe problem in the reproductive health field, the Fund’s area of focus. The vast majority of Afghan women go through pregnancy and childbirth with no skilled assistance. In rural Afghanistan, NGOs run most of the existing maternal and child health centres.
Other NGOs active near Mazar-i-Sharif include the Swedish Committee for Afghanistan and IbnSina. Both groups have been providing services including reproductive health care for years, but have stepped up their activities and now run numerous clinics. UNFPA provides supplies, including kits for clean deliveries at home, where most Afghan women give birth, and family planning commodities. It also funds training of medical staff, helping address the severe shortage of health professionals, especially females, available in rural areas.
IbnSina operates an emergency obstetric care and training facility in Langalkha, between Mazar-i-Sharif and the ancient city of Balkh. Traditional birth attendants (TBAs) in 11 surrounding villages have been trained to refer complicated deliveries to the centre.
Early one July morning Langalkha’s waiting room is filled with women in white burkas holding small children in their laps. In the next room, a health educator is teaching a dozen women about hygiene. In another room equipped for deliveries, a female doctor examines a young woman who came in after suffering a miscarriage.
TBAs and volunteer community health workers from nearby villages have come to the clinic to meet some international visitors. In a training room, one TBA uses an infant dummy to demonstrate post-delivery procedures as 10 others look on.

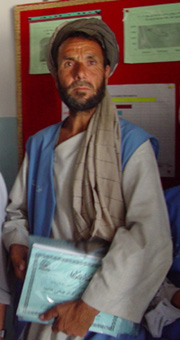
Some of the male health workers talk about their educational activities. Besides teaching about sanitation, hygiene and vaccination of children, they give information about family planning and the benefits of having small families. One of the older men in the group says villagers are receptive to these messages; when asked about his own children he laughs and says he has seven.
The Swedish Committee also has a clinic in Balkh providing maternal and child health services and emergency obstetric care, for the time being. The government has asked the group to move the facility to a more remote area that lacks services. The clinic is staffed by three doctors (two are female), a health worker, a pharmacist, a receptionist and three community health workers responsible for patient education. The delivery room is always available for emergency cases and a doctor is on call 24 hours a day.
Six supervisors manage 42 TBAs in the clinic’s catchment area. “The TBAs are the bridge between us and the community. If they can’t help, they will send people to the clinic,” says Dr. Abdul Qadeer, health manager for the Swedish Committee’s northern regional office.
Dawn Laboc, a nurse midwife from the United States, is visiting the Balkh clinic. She is one of three UNFPA-funded international maternal and child health advisers helping the Swedish Committee improve its training and supervision of reproductive health service providers. “I go to the clinics over and over, to check delivery equipment and supplies and see how the place is functioning,” she says.
Looking at the work of TBAs and their supervisors “is the creative aspect of my job,” she states. “I will often gather 21 of them together to see what their practices are and whether they are beneficial or harmful.” The system is not ideal; TBAs at best receive only very limited training, and may not know how to deal with difficult cases. “I’ve had TBAs tell me that when a baby isn’t breathing, they throw cold water on it. This creates hypothermia, which leads to hypoglycaemia and the baby gets further depressed.” There can also be jealousy between the paid supervisors and the unpaid TBAs.
TBAs help compensate for the severe scarcity of female doctors and midwives, especially in rural areas, but their effectiveness in reducing maternal mortality is not clear. For now, the Swedish Committee is providing refresher training for existing TBAs but is not training new ones. A main point of the training is to reduce delays in referring complicated deliveries to the clinic.
“I’ve seen some cases referred way too late,” Laboc says. “When I go to refresher trainings, I emphasize that if the TBA thinks there is a problem and the patient or her family doesn’t want to go to a referral facility—because they don’t have the money for transportation, or it’s raining or they don’t have someone to take care of the children—if they don’t go now, they may get referred when it’s too late.”
Many rural Afghan women who experience life-threatening problems such as prolonged labour post-partum haemorrhage or hypertension have little hope of referral. “We have many parts in this country with no means of transport or roads,” Dr. Qadeer notes. From some villages in mountainous Badakhshan province, he says, clinics can only be reached by horse or donkey and the nearest emergency obstetric care centre is three days away.
This points up the ongoing challenges facing Afghanistan despite recent gains. “There are problems everywhere you turn, so many it’s hard to know which to attack,” states Laboc.
“Should we focus limited resources on TBA refresher training and supervision in the regions accessible to a referral system, for maximal impact on reducing maternal and infant mortality and morbidity? Or should we focus on rural regions where TBA practice is not well supervised and there are no adequate referral resources? These village women desperately need education and supplies to provide the safest deliveries possible in conditions where there are no other options.”
-William A. Ryan